Each year, 60 million Americans experience mental illness. Across the United States, each year, regardless of race, age, religion, or economic status, mental illness affects the lives of one in four adults and one in 10 children. This means that someone in every family has mental illness.
Most of our patients probably don’t tell anyone that they or one of their family members has mental illness They probably are doing what most of us do: Pretend it’s not there. Why? Because the stigma of mental illness is pervasive and destructive. What can we do to decrease the stigma?
The word stigma is derived from Greek and means "to mark the body." The bearer of the mark, or the stigma, is avoided and shunned. This practice has continued through the ages. In medieval times, if a person had a mental illness, he or she was thought to be possessed by demons and viewed as weak. Today, people with mental illness are viewed as menacing, deviant, unpredictable, incompetent, or even dangerous. It is entirely reasonable then, that we would want to avoid the stigma of mental illness. However, this prejudice against mental illness must be challenged.
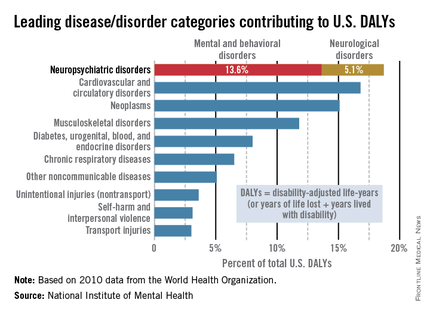
Mental illness accounts for increased morbidity and mortality as well as lifetime disability. The World Health Organization (WHO) estimates that neuropsychiatric disorders are the leading cause of disability in the United States, followed by cardiovascular and circulatory diseases, and neoplasms. The neuropsychiatric disorders category, which includes mental and behavioral disorders, accounts for 13.6% of total U.S. disability-adjusted life years (DALYs). Neurological disorders account for 5.1% of total U.S. DALYs.
Impact on the family
Not only does stigma affect individuals, it affects family members as well. Family members suffer from SBA, or stigma by association (Brit. J. Psych. 2002;181:494-8), also known as courtesy stigma (Social. Psychiatry Psychiatr. Epidemiol. 2003;38:593-602). Families share stigma because families share a genetic heritage. Families share stigma by assuming responsibility for their family members’ behaviors. Families share stigma because they are seen as having common motivations (J. Pers. Soc. Psychol. 2012;102:224-41).
SBA causes psychological distress in family members (Rehabil. Psychol. 2013;58:73-80; J. Nerv. Ment. Dis. 1987;175:4-11; Br. J. Psychiatry 2002;181:494-8; and Schizophr. Bull. 1998;24:115-126).
Psychological complaints, such as brooding, inner unrest, and irritability, and physical complaints, such as insomnia, fatigue, and neck and shoulder pain, have been attributed to the psychological distress of SBA. Family members may avoid social interactions and conceal their relationship to the family member who is mentally ill (Acad. Psychiatry 2008;32:87-91). They might psychologically distance themselves from a relative with mental illness.
SBA varies by disease type, family role, and age. The greatest SBA is associated with drug dependence. These family members are blamed for the illness, held responsible for relapse, and viewed as incompetent. In the study of Patrick W. Corrigan, Psy.D., (J. Fam. Psychol. 2006;20:239-46), family members report feelings of "contamination" and shame. Severe depression or panic and phobias engender less stigma. More educated people are less likely to report feelings of stigma.
According to Dr. Corrigan, SBA varies by family role: Parents are blamed for causing the child’s mental illness, siblings are blamed for not ensuring that relatives with mental illness adhere to treatment plans, and children are fearful of being "contaminated" with the mental illness of their parent. The closer the relationship, the less the stigma is perceived as defining the person. Family closeness can reduce stigma (The Gerontologist 2012;52:89-97). Regarding age, a British study showed that the highest stigma is reported in the 16- to 19-year-old age group (Br. J. Psychiatry 2000;177:4-7).
Psychiatry as a profession has not helped diminish stigma. It is not uncommon to hear psychiatrists assign blame to parents or spouses. Psychiatrists often believe that the family has a role in the patient’s illness. How many spouses have been told they are "codependent" with the implication that they have somehow "caused the illness"? What can we do diminish stigma?
Fighting stigma
Fighting stigma means confronting stigma (Advances in Psychiatric Treatment 2000;6:65-72). Most efforts worldwide have begun with the idea of educating people about mental illness. These efforts, focused on promoting mental illness as a biological illness, have had limited success and in some situations actually increased stigma (Acta Psychiatr. Scand. 2012; 125:440-52). The answer may lie in targeted education: specific facts for specific groups.
For example, young couples with children become less fearful after education targeted specifically for them (Br. J. Psychiatry 1996;168:191-8). Antistigma campaigns are common throughout the world. The websites of most professional psychiatric organizations, such as the American Psychiatric Association, the Royal College of Psychiatrists, and the College of Psychiatrists of Ireland, provide information about antistigma campaigns. Organizations often partner with mental health charities. Antistigma efforts also focus on publishing articles about stigma as the Lancet did in a series a few years ago (1998;352:1048). It is unclear whether these efforts reduce stigma. Dr. Corrigan suggests that meeting people who have mental illness weakens the tendency to link mental illness and violence (Psychiatric Rehabilitation Skills 2002;6: 312-34).