Princeton University Professor of Economics and Public Affairs Anne Case, Ph.D., and 2015 Nobel Prize winner in economics Angus Deaton, Ph.D., recently made headlines with an article in the Proceedings of the National Academy of Sciences that showed a remarkable anomaly in global death rates.
The steady decline in death rates seen across the world for age-specific cohorts held true in the United States with one exception: White men and women aged 45-54 years and only in the period of 1999 to 2013. The rising death rates in this cohort were concentrated most intensely among those with less than a high school education and among men. This finding was not seen in cohorts from other countries or in this age group in the United States before 1999.
Many explanations have been given for this focused finding, from income inequality to the stubbornly slow recovery from the recent economic recession. But none of these speculations explains why the upturn in death rates was not seen among Hispanics or blacks in this age cohort – or why it was not seen in the decade before 2000.
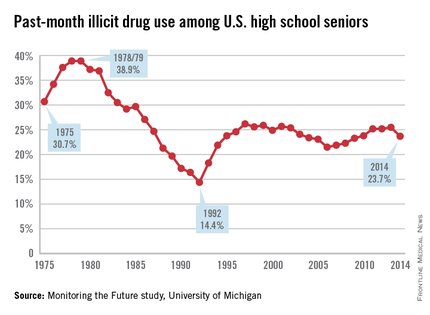
Several clues provide insight. The first is that the increase in deaths was mostly the result of rising rates of drug overdose, suicide, and chronic liver disease, including cirrhosis of the liver. In 1978, the peak of the modern drug epidemic, this cohort was aged 10-24 years. This sharp drug abuse epidemic was distinctly American and more prevalent among white males than among white females or other males. The annual Monitoring the Future study, funded by the National Institute on Drug Abuse and conducted by the University of Michigan, Ann Arbor, has chronicled the patterns of substance use for American 12th graders from 1975 to the present. It provides a snapshot of the patterns of adolescent drug use in this cohort. During the peak of the national drug epidemic, this cohort was at the most vulnerable age for starting drug use.
The second clue to this puzzle is that in recent decades, there has been a breakdown in the health and social capital of whites having lower educations, as author and political scientist author Charles Murray, Ph.D., recounted in a recent book (“Coming Apart: The State of White America, 1960-2010,” [New York: Crown Forum, 2012]). This might have resulted in an increased vulnerability in midlife within this cohort to adverse health effects and in less resiliency in mitigating those effects.
A third relevant clue is that the adverse health effects of adolescent drug use are not limited to adolescence. Substance use disorders most commonly begin in the teenage years (Nature. 2015 Jun;[522]:S46-7). Early drug use is a predictor of lifelong serious co-occurring health problems, including addiction to alcohol and other drugs.
Thus, in addition to the explanations already put forth in response to the Case-Deaton findings, an additional factor has significance. The leading edge of the Baby Boom generation not only sparked the modern drug abuse epidemic in their teen years but also carries with it a substantially heightened lifelong health risk for overdose death, suicide, and chronic liver disease.
This finding is significant not only for the health of this aging cohort but also for young people today. The delayed consequences of adolescent drug and alcohol use provide another good reason to refocus public health efforts to encourage youth to grow up without using alcohol, tobacco, marijuana, and other drugs.
Dr. DuPont is president of the Institute for Behavior and Health, Rockville, Md., and was the first director of the National Institute on Drug Abuse (1973-1978).