Recent examples come quickly to mind:
• $100 million from the Lieber family to fund the Lieber Institute for Brain Development at Johns Hopkins University
• $300 million from Microsoft co-founder Paul G. Allen to create the Allen Institute for Brain Science
• $650 million from Ted Stanley for the Stanley Center at the Broad Institute.
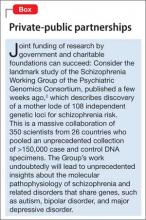
Such generosity is cause for celebration by psychiatrists and their long-suffering patients who are disabled by a brain disorder. Private money supplements research funding by the National Institutes of Health and will bolster the war against mental illness,1 which costs >$300 billion annually (Box,2page 12).
Although philanthropy will help, many needs in psychiatry are unmet, and not all can be addressed with money. Consider a number of areas of need.
Unmet clinical needs
Models of disease. Psychiatry is in desperate need of an objective, valid diagnostic system that transcends the DSM model of symptom clusters. The Research Domain Criteria3 represents the effort to find an alternative. To achieve that goal, it’s necessary to identify biomarkers and establish their utility—a task that requires a huge amount of funding.
Therapeutics. Clinicians are hungry for innovative, safe pharmaceuticals and non-drug treatments that modify disease, not just alleviate symptoms. Obsessive-compulsive disorder always has lacked such therapies; so have dementia, schizophrenia, personality disorders, dissociative disorders, and sexual pathologies. In fact, >80% of DSM disorders do not have an FDA-approved, evidence-based treatment,4 and many available medications are only partially efficacious, poorly tolerated, or unsafe.
There are more unmet needs in therapeutics:
• Development of promising non-drug therapies, such as neuromodulation, proceeds slowly.
• Research into neurobiological mechanisms of psychotherapy is in its infancy.
• A foolproof method to monitor adherence does not exist, and countless patients relapse needlessly and deteriorate functionally.
• Effective, evidence-based rehabilitation for serious psychiatric disorders is used narrowly and vastly underfunded.
• Insurers continue to thumb their nose at laws that require parity for treating mental illness—thus impeding access to, delaying, or truncating psychiatric care.
Unmet scientific needs
Translational investigators. Despite increased funding for basic neuroscientific study and breathtaking discoveries in animal molecular neurobiology, a trickle of findings has been applied to clinical medicine. This translational gap has many causes, including a shortage of translational neuroscientists (MD-PhD psychiatrists and neurologists), insufficient long-term funding to develop such clinician-researchers, and complex regulatory oversight of human research.
Stalled progress in drug development. Development of novel-mechanism therapeutics for brain disorders is languishing. Some pharmaceutical manufacturers have abandoned the development of drugs that act on the CNS in favor of less complex, more lucrative areas such as oncology and cardiology; others have reduced their investment in CNS products. Developing treatments for knotty disorders of the most complex structure in the known universe requires mammoth investment. Why are stakeholders bailing out on the greatest challenge for science and medicine for easier endeavors?
Discovering new genes for every devastating neuropsychiatric syndrome, such as schizophrenia, is cause for celebration, but the champagne won’t flow until the coding of every gene is unscrambled so that specific biological interventions can be developed. The cost of the chase might be orders of magnitude greater than what is invested in research today. Conceptualizing new models of brain disorders is a critical part of scientific progress and an antidote to the inertia of perpetual group-think. Depression, for example, is being reconceptualized as a disorder of impaired neuroplasticity and neurotropic deficiency, rather than a shortage of serotonin and norepinephrine. Rapid reversal of severe depression to euthymia—in 1 or 2 hours—with IV ketamine shattered the dogma that depression takes weeks to lift, and is ushering in unprecedented new thinking and models likely to revolutionize treatment of severe depression. We need such breakthroughs for other psychiatric brain disorders.
Unmet professional and sociopolitical needs
Broadening of training. Psychiatrists have focused on the mind but insufficiently attended to the biology of the brain. For psychiatry to rise to the next level as a medical specialty and brain discipline, training must incorporate more neurology than it does now. The converse is true in neurology.
Hospitalization not incarceration. It is unconscionable that people suffering from a medical illness that impairs their judgment and behavior are locked up as criminals. Psychiatry must forcefully lobby so that the seriously mentally ill are treated in secure hospitals staffed by physicians, nurses, and mental health professionals.
That’s right: Bring back the asylum to address this unmet medical, political, and ethical need for psychiatric patients.a A serious mental disorder must be accepted as a fault-free illness.
aTo read more about this, I recommend my March 2008 editorial, “Bring back the asylums?,” at CurrentPsychiatry.com, and Dr. George Paulson’s excellent book, Closing the asylums: Causes and consequences of the deinstitutionalization movement (Jefferson, NC: McFarland & Co. Inc; 2012).